

L'apnée et la respiration irrégulière concernent presque tous les prématurés et les nouveau-nés. Plus le bébé est prématuré, plus l'apnée est marquée. Il s'agit d'une perturbation de la mécanique respiratoire et du contrôle respiratoire. La caractéristique la plus importante de l'apnée est le débit d'air intermittent dans les voies aériennes du patient.
L'apnée est cliniquement significative pour le patient en raison des symptômes concomitants comme la bradycardie < 80 bpm (fréquence cardiaque diminuée) et l'hypoxie < 80 % (saturation en oxygène diminuée). L'objectif de la prophylaxie et du traitement de l'apnée est d'éviter et limiter les effets négatifs (
Les cycles respiratoires supplémentaires stimulent la respiration
Les voies aériennes sont stabilisées, ce qui facilite la respiration
Le propre cycle respiratoire du patient est détecté et le dispositif passe en mode CPAP
Disponible avec les dispositifs medinCNO, medinCNOmini, medin-NC3
Les études confirment l'efficacité de la CPAP nasale dans ce contexte. Cet élément fait partie des recommandations actuelles pour le traitement de l'apnée et de ses symptômes concomitants (
Les mécanismes d'action sont les suivants :
Le mode ApnéeCPAP de medin comme traitement de l'apnée peut être utilisé de la prophylaxie au traitement d'une apnée avérée.
En mode nCPAP, l'apnée centrale et l'apnée obstructive sont détectées grâce à la technologie unique MediTRIG et traitées par des cycles respiratoires supplémentaires automatiques du dispositif de CPAP. Le niveau de pression de pointe des cycles respiratoires est ajusté avec un deuxième débitmètre électronique et ajouté au débit de base. Les paramètres de la fonction ApnéeCPAP et de la technologie MediTRIG peuvent être adaptés à chaque patient.
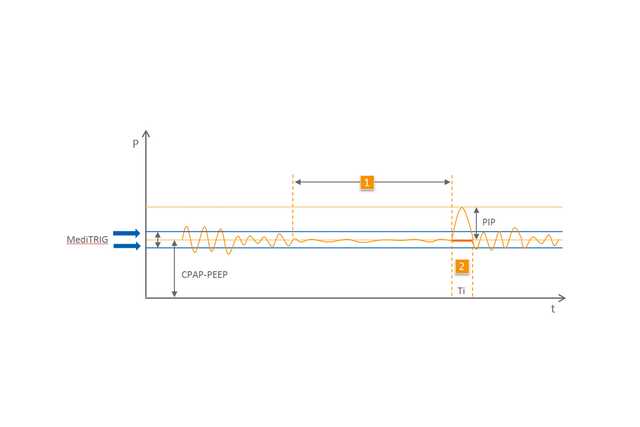
1 Apnée
2 Cycle respiratoire automatique