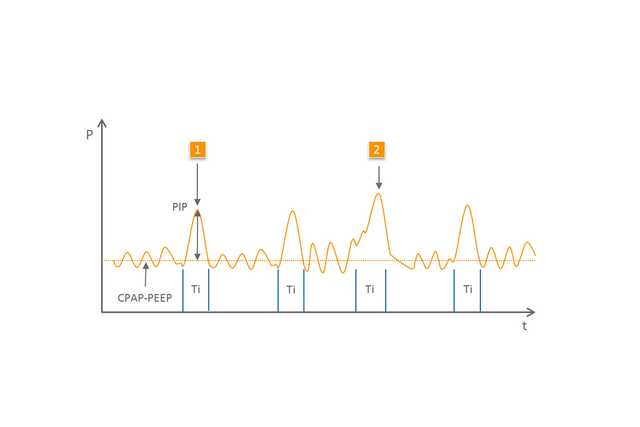
NIPPV es un término genérico que abarca diversos métodos de ventilación en los que, además de utilizarse la CPAP/PEEP, se aplican respiraciones controladas para proporcionar soporte al paciente. El nivel de presión de estas respiraciones es mayor y no se emiten de manera sincronizada. Se han establecido ciertas diferencias entre las distintas variantes de este método de soporte respiratorio (
Dentro de este grupo, la NIPPV (
Soporte respiratorio controlado para neonatos
Soporte eficaz tras la extubación y durante la apnea (1,2)
Fácil de usar y ajustar
Disponible en los dispositivos medinCNO, medinCNOmini y medin-NC3
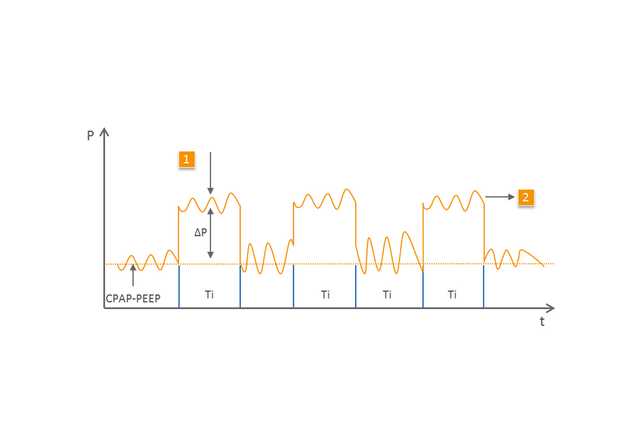
El modo BiLevel (
1 Respiración mecánica
2 Respiración espontánea en el segundo nivel de presión más alta
Los efectos y la eficacia de la NIPPV han sido objeto de investigación en numerosos estudios (
Los dispositivos CPAP especializados de medin, combinados con el generador de nCPAP Medijet son idóneos para su uso con los modos de ventilación NIPPV y BiLevel. Con el flujo básico, el paciente puede recibir la CPAP/PEEP deseada. Con la ayuda de un segundo nivel de flujo, que se suma al flujo básico y se define a través de un medidor de flujo electrónico adicional, Medijet genera un nivel de presión más alta.
Dado que Medijet permite realizar la expiración en cualquier momento, el paciente puede respirar libremente con cualquiera de estos niveles de presión. Gracias a esto, los dispositivos CPAP de medin ofrecen todas las opciones de soporte respiratorio con NIPPV.