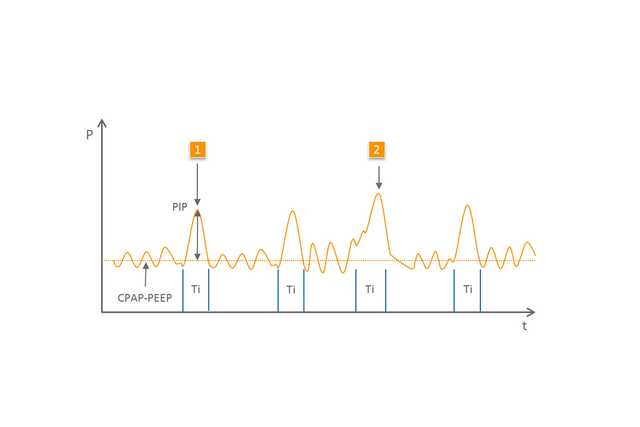
Der Oberbegriff NIPPV (Nasal Intermittend Positive Pressure Ventilation, nasale intermittierende Positivdruckbeatmung) umfasst Modi, bei denen – zusätzlich zum CPAP/PEEP – kontrollierte Atemhübe zur Unterstützung des Patienten verabreicht werden. Diese Atemhübe haben ein höheres Druckniveau und werden nicht synchronisiert abgegeben. Zwischen den unterschiedlichen Varianten dieser Form der Atemunterstützung wird differenziert (
NIPPV (
Kontrollierte Atemunterstützung für Neonaten
Wirkungsvolle Unterstützung nach der Extubation und während Apnoe (1,2)
Bedienfreundlichkeit und einfache Anpassung
Verfügbar bei den Geräten medinCNO, medinCNOmini, medin-NC3
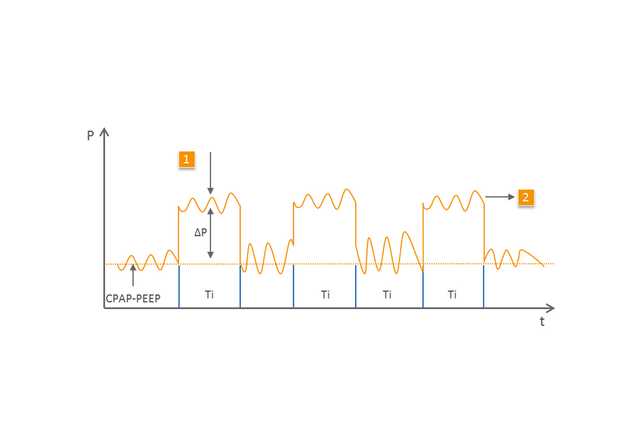
Der BiLevel-Modus (
1 Maschineller Atemhub
2 Spontanatmung auf dem zweiten, höheren Druckniveau
Die Auswirkungen und Wirksamkeit der NIPPV wurden in zahlreichen Studien untersucht (
Die spezialisierten CPAP-Geräte von medin in Verbindung mit dem Medijet nCPAP-Generator sind ideal für den Einsatz von NIPPV und BiLevel geeignet. Beim Basisflow wird der Patient mit dem gewünschten CPAP/PEEP versorgt. Mithilfe eines zweiten Flowniveaus, das zusätzlich zum Basisflow über ein weiteres elektronisches Flowmeter eingestellt wird, erzeugt Medijet ein höheres Druckniveau.
Da Medijet zu jeder Zeit die Exspiration zulässt, kann der Patient bei beiden Druckniveaus frei atmen. Dadurch ermöglichen die medin CPAP-Geräte alle Optionen der NIPPV-Atemunterstützung.